
What is Type 2 Diabetes?
Diabetes is a complex disease that disrupts the body’s ability to effectively process sugar and convert it into energy. Blood glucose ( more commonly known as blood sugar) is your main source of energy and comes from the food you eat. Insulin, a hormone made by the pancreas, helps glucose from food get into your cells to be used for energy. In Type 2 diabetes the insulin isn’t able to get the food into your cell, resulting in elevated blood sugars.
What is happening in your body with Type 2 Diabetes?
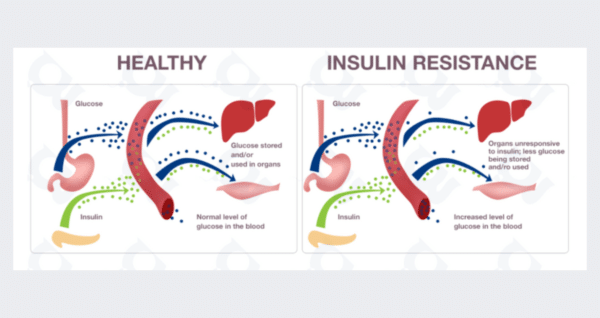
Either the pancreas fails to produce enough insulin or the body becomes resistant to insulin. As a result, glucose remains in the bloodstream instead of being transported into the cells where it is needed for energy, creating high blood sugar levels. This prolonged elevation of sugar levels can have detrimental effects on various organs and systems in the body.
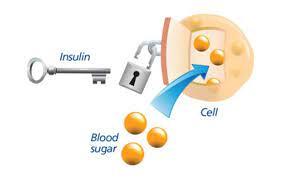
Pictured above is a great visual of what is happening. Insulin is the key that will open the lock on cell “doors” to allow blood sugar in to use for energy. There are either not enough “keys” (insulin) being made or they aren’t able to fit in the lock. This leaves the sugar in the blood stream.
What causes Type 2 Diabetes?
There is still ongoing research but the main factors include:
- Genetic Susceptibility
- Lifestyle- diet and exercise
- Aging- beta cell decreases with age
- Medications
Social determinants of health can also have an effect on type 2 diabetes development from access to healthcare, appropriate education, and more.
What is Insulin Resistance?
Insulin resistance refers to a condition where the body’s cells become less responsive to the effects of insulin, leading to elevated blood sugar levels. Insulin resistance has a significant impact on glucose metabolism, as it impairs the ability of cells to take up glucose, resulting in increased blood sugar levels.
Several factors contribute to the development of insulin resistance. Genetic predisposition, sedentary lifestyle, poor diet, medications, inflammation, and hormones (particularly in pre-menopausal women) are all contributing factors.
Health Complications
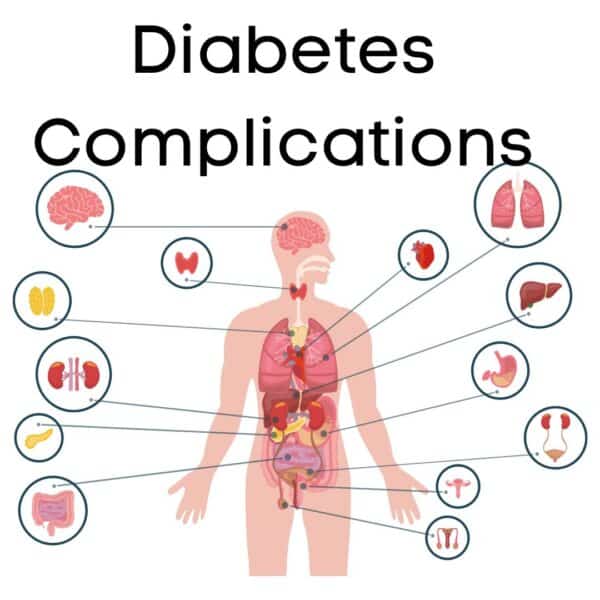
High blood sugar over a long period of time can lead to long term complications in your kidneys, eyes, nerves, and heart.
Kidney damage
High blood glucose can damage the blood vessels in the kidneys. The damaged blood vessels cannot filter all the waste products from your blood, so some waste remains in your blood. To detect kidney disease a urine test should be performed annually.
Eye problems
Retinopathy is the eye problem that diabetes causes most often. The blood vessels in the retina of the eye become damaged. It’s important to have a dilated eye exam every year.
Nerve problems
High blood glucose damages the nerves. Nerve damage, or neuropathy, usually happens in the feet and lower legs because blood flow to the end of the body is poor. You may get numbness, tingling, pain, or loss of feeling. Daily foot care is very important to prevent sores. Nerve damage can also cause sexual problems, stomach, and/or bladder issues as well.
Heart problems
Adults with diabetes are nearly twice as likely to have heart disease or stroke as adults without diabetes. High blood glucose can damage blood vessels, making it difficult for blood to reach all parts of the body. A person with diabetes can reduce the risk of heart and blood vessel disease by knowing the “ABCs” of diabetes.
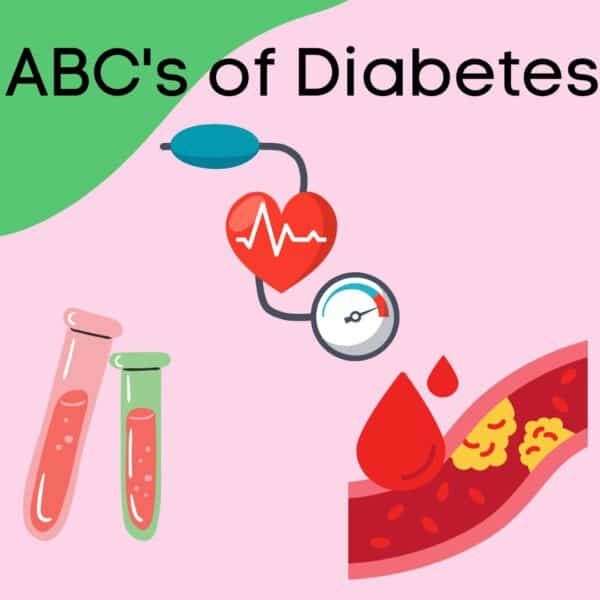
- A is for A1C-a test that measures your blood glucose control over the past 3 months.
- B is for Blood Pressure-blood that pushes too hard against artery walls makes your heart work harder, causing higher blood pressure
- C is for Cholesterol– Diabetes tends to lower “good” cholesterol levels and raise triglycerides and “bad” cholesterol levels, which increases the risk for heart disease and stroke. High LDL (low-density-lipoprotein) levels can contribute to narrowed or blocked arteries that can ultimately lead to heart attack or stroke.
| Blood Test | Pre-Diabetes Diagnosis | Diabetes Diagnosis |
| Fasting Plasma Glucose | 100-125 mg/dl | 126 mg/dl or higher |
| Oral Glucose Tolerance Test | 140-199 mg/dl | 200 mg/dl or higher |
| A1c | 5.7% – 6.4% | 6.5% or higher |
Understanding Diagnostic Criteria:
There are a few different tests used to diagnose diabetes. The most commonly used test is the measurement of fasting plasma glucose levels. A fasting plasma glucose test involves measuring blood sugar levels after you have fasted for a certain period, usually overnight. A fasting plasma glucose level of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions confirms the diagnosis of type 2 diabetes.
HbA1c testing measures the amount of hemoglobin with sugar attached. By measuring this percent, your average blood sugar levels over the past two to three months can be determined . An HbA1c level above 6.5 indicates the presence of diabetes. Normal A1c is under 5.7 percent and pre-diabetes diagnosis is 5.7-6.5%.
Diabetes management- The Signature 6 M Method
We will dive into each “M” of my signature 6 M Method and set up the framework for lifelong diabetes self management.
The 6 M Method helps you be:
- Empowered by understanding diagnosis
- Knowledgeable of how to balance meals/snacks
- Understand behaviors are more important than weight
- Grow confidence in using lifestyle changes to manage diabetes
Monitoring
This includes regular doctor performed tests as well as at home monitoring. Important data collected is used to make decisions about treatment and understand the current state of your diagnosis. This includes:
- Goal ranges
- Being aware of low blood sugar and treatment options
- ABC’s- A1c, Blood Pressure, Cholesterol Labs
- Lab work and annual testing: UACR, DRE, Lipid profile, and more
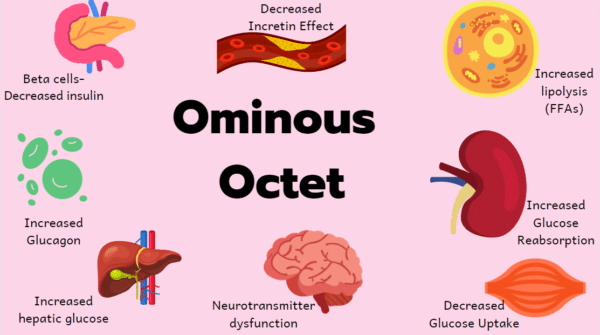
Medication
Medication helps target the core defects that type 2 diabetes creates in the body. These defects are referred to as the “Ominous Octet” which addresses different parts of the body including:
- Pancreas-decreased insulin secretion
- Gut- (small intestine) decreased incretin effect increased lipolysis- insulin inhibits lipolysis (breakdown of fats)- more free fatty acids can lead to more insulin resistance (and weight gain)
- Kidneys-increased glucose reabsorption
- Muscles- decreased glucose uptake
- Brain-neurotransmitter dysfunction
- Liver- increased hepatic glucose production, and increased glucagon secretion
(I also addressed diabetes supplements in another blog post if you are interested in learning more!)

![]()
Meals
All the food you eat and drink are broken down in the body, carbohydrates break down into glucose (simple sugar molecules). The type and amount of carbohydrates you consume affect the blood sugar, the carbs in some foods (mostly those that contain a lot of simple sugars) cause the blood sugar level to rise more quickly than others. How fast or slow carbohydrates are turned into blood glucose are measured on the glycemic index.
Everyone’s body responds differently to different types of foods and diets, so there is no single “magic” diet for diabetes. But you can follow a few simple guidelines to find out what works for you to help manage your blood sugar. I’ll detail this more in another post but I do have a free ebook on carb pairing so make sure you grab your copy now. And check out some of my posts on best fast food breakfast for diabetes, low carb soups for diabetics, best protein bar, healthy packaged snacks for diabetes, and my recipe library.

Movement
Exercise helps by making you more sensitive to insulin and this response lowers blood sugars. You don’t have to join a gym to get the activity you need. Even everyday activities can make a difference like cleaning the house, walking, taking the stairs, etc.
The most important thing you can do is find exercise that feels best for you that you really enjoy. Both cardio and strength training are beneficial- you can try biking, Zumba, lifting weights, yoga, tai chi, swimming, dancing, karate, and more.

Mindset
Diabetes distress is what some people feel when they’re overwhelmed by the relentlessness of diabetes. This can lead to diabetes burnout and stress.
Stress leads to higher cortisol. Chronic stress causing higher cortisol can lead to elevated blood sugars. Stigma (such as diabetes stigma) is a form of chronic stress. The increased cortisol production (stress) leads to increased blood sugars- stress affects glucose levels and there is often additional stress for patients who experience stigma around their bodies and their diagnosis.
Stress management and self care are important to keep blood sugars well controlled. You can practice self care in many different ways including meditation, deep breathing, exercise, reading, listening to music, calling a friend, going for a walk, playing games, coloring- really whatever helps you relax!
Maintenance
Many diabetes care guidelines are weight and weight-loss focused. These counseling messages are problematic and may contribute to disordered eating, shame, and/or weight stigma.
By setting non-weight focused goals and creating self-care behaviors such as adding in nutritious foods, eating mindfully to honor hunger and fullness, getting regular movement that you love, improving sleep and managing stress.
A large body of scientific evidence shows that behaviors have a much bigger impact on health than weight alone, and easier to maintain long term. So put your focus into the 6 M Method for successful diabetes management. Learn more about the method and how you can work with me to lower your A1c on my services page.




Pingback: Best Packaged Snacks for Diabetics
Pingback: A1c Conversion | Dietitian Jess Nutrition - Accent Meal
Pingback: Best Sugar Substitute for Diabetes: Allulose - Accent Meal
Pingback: Best Low Carb Options for Diabetics at Subway - Accent Meal
Pingback: Todo lo que necesitas saber sobre la diabetes tipo 2 - HealthierLife